More Information
Submitted: August 25, 2022 | Approved: September 12, 2022 | Published: September 13, 2022
How to cite this article: Zhukov KV, Gasparuan BA, Vetcher AA, Shishonin AY. Centralized aerobic-anaerobic energy balance compensation theory perspective in biomedicine. Arch Biotechnol Biomed. 2022; 6: 007-009.
DOI: 10.29328/journal.abb.1001031
Copyright License: © 2022 Zhukov KV, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Centralized aerobic-anaerobic energy balance compensation theory perspective in biomedicine
Kirill V Zhukov1, Bagrat A Gasparuan1, Alexandre A Vetcher1,2* and Alexander Y Shishonin1
and Alexander Y Shishonin1
1Complementary and Integrative Health Clinic of Dr. Shishonin, 5 Yasnogorskaya Street, Moscow, 117588, Russia
2Peoples’ Friendship University of Russia (RUDN), 6 Miklukho-Maklaya Street, 117198 Moscow, Russia
*Address for Correspondence: Alexandre A Vetcher, Complementary and Integrative Health Clinic of Dr. Shishonin, 5 Yasnogorskaya Str, Moscow, 117588, Russia, Email: [email protected]
Recently announced centralized aerobic-anaerobic energy balance compensation (CAAEBC) theory has already demonstrated achievements in the treatment of arterial hypertension (AHT), diabetes myelitis (DM) and osteochondrosis. Such demonstration lifts the necessity to check the applicability of this theory to other non-communicable diseases (NCDs) and develop the proper way to model the main idea of CAAEBC.
For a while the etiology of essential AHT was unclear. Namely, this is a reason why it was called essential by Mahomed and Frank in 1911 [1]. Even several years ago the scientific community felt that the knowledge about detailed mechanisms of conversion of pre-AHT to AHT was far from understood [2]. It needs to be underlined, that for a while the observations that AHT correlates with the brachiocephalic arterial blood flow issues existed. The vast majority of authors acknowledged statistical correlation [3-5]. As a matter of fact, we were able to find a single report, where AHT was considered a result of the obstructions of blood access to the brain [6].
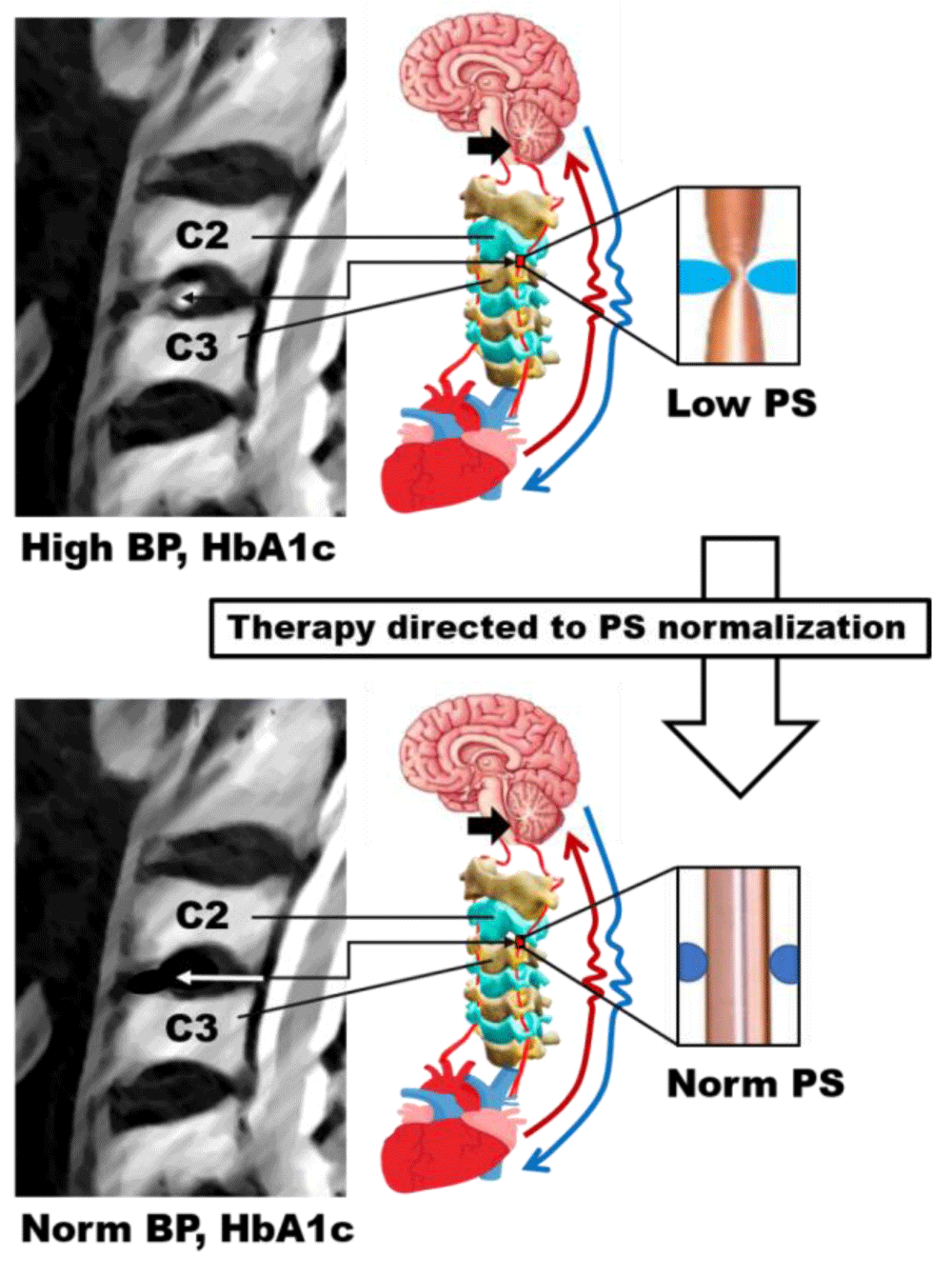
Recently we explained through the development of CAAEBC theory why the access of arterial blood flow to the rhomboid fossa is so critical to the body internal conditions regulation [7]. The visual explanation is exhibited in Figure 1. So far, we have demonstrated, that the proposed approach helps the body regain control of arterial blood pressure (BP) [8], HbA1c [9] and vertebral cartilage [10]. Following the above-mentioned, let’s discuss the directions of consecutive steps to find a place for CAAEBC theory in the garden of contemporary therapy.
Figure 1: The summary of the available data of CAAEBC theory applications to AHT, DM and osteochondrosis [7-10]. Black arrow indicates rhomboid fossa. The Systolic peak (PS) represents the linear velocity of the blood flow.
CAAEBC theory suggests that the restoration of the above-mentioned access with the subsequent strengthening of the cervical muscular corset will eventually lead to the normalization of the majority of internal body functions and therefore, parameters. Of interest is to understand which parameters are easy to acquire to start with them. It seems that in addition to BMI [11] and SaO2 [12,13] it will be easy to obtain pH data. Indeed, pH measurements are very important for the following reasons:
- According to modern Medicine, maintaining acid-base balance is an indicator of a good health
- CAAEBC theory directly connects certain NCDs with changes in blood pH [7,10].
But it appears that there are some restrictions on its acquisition and interpretation [14]. Therefore, a procedure for blood pH measurements needs to be developed.
Another issue is the necessity to step from medical record analysis to the experiment. The best options to collect experimental data are definitely animal models, but available sources do not allow us to choose the best specie [15-23].
We demonstrate, that next steps to prove CAAEBC theory should be
- Analysis of BMI and SaO2 data
- Development of the procedure to collect blood pH data
- Introduction for appropriate animal model
Author Contributions
Conceptualization, A.Y.S., A.A.V., B.A.G., A.Y.S.; writing—original draft preparation, A.Y.S., A.A.V.; writing—review and editing, A.Y.S., A.A.V.; visualization, A.A.V.; supervision, A.Y.S. and A.A.V.; project administration K.V.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This paper has been supported by the RUDN University Strategic Academic Leadership Program (recipient A.A.V).
The authors wish to thank BS V.D. Bystrykh for her assistance with the editing of the submission’s final version. Alexandre Vetcher expresses acknowledgments to the RUDN University Strategic Academic Leadership Program for the obtained support.
- Kotchen TA. Historical trends and milestones in hypertension research: a model of the process of translational research. Hypertension. 2011 Oct;58(4):522-38. doi: 10.1161/HYPERTENSIONAHA.111.177766. Epub 2011 Aug 22. PMID: 21859967.
- Whelton PK, Einhorn PT, Muntner P, Appel LJ, Cushman WC, Diez Roux AV, Ferdinand KC, Rahman M, Taylor HA, Ard J, Arnett DK, Carter BL, Davis BR, Freedman BI, Cooper LA, Cooper R, Desvigne-Nickens P, Gavini N, Go AS, Hyman DJ, Kimmel PL, Margolis KL, Miller ER 3rd, Mills KT, Mensah GA, Navar AM, Ogedegbe G, Rakotz MK, Thomas G, Tobin JN, Wright JT, Yoon SS, Cutler JA; National Heart, Lung, and Blood Institute Working Group on Research Needs to Improve Hypertension Treatment and Control in African Americans. Research Needs to Improve Hypertension Treatment and Control in African Americans. Hypertension. 2016 Nov;68(5):1066-1072. doi: 10.1161/HYPERTENSIONAHA.116.07905. Epub 2016 Sep 12. PMID: 27620388; PMCID: PMC5063700.
- de Simone G, Mancusi C, Esposito R, De Luca N, Galderisi M. Echocardiography in Arterial Hypertension. High Blood Press Cardiovasc Prev. 2018 Jun;25(2):159-166. doi: 10.1007/s40292-018-0259-y. Epub 2018 May 2. PMID: 29721914.
- Finocchi C, Sassos D. Headache and arterial hypertension. Neurol Sci. 2017 May;38(Suppl 1):67-72. doi: 10.1007/s10072-017-2893-x. PMID: 28527058.
- Wermelt JA, Schunkert H. Management der arteriellen Hypertonie [Management of arterial hypertension]. Herz. 2017 Aug;42(5):515-526. German. doi: 10.1007/s00059-017-4574-1. PMID: 28555286.
- Ermoshkin VI. [Hypothesis of causeless hypertension.] (In Russian) http://www. medlinks.ru/. 2011.
- Vetcher AA, Zhukov KV, Gasparuan BA, Shishonin AY. The cerebellum role in arterial hypertension. Medical Hypotheses. 2022; 162:10835 doi:10.1016/j.mehy.2022.110835
- Vetcher AA, Zhukov KV, Gasparuan BA, Shishonin AY. The cervical blood flow parameters with the best correlation from arterial blood pressure in hypertension cases International Journal of Recent Scientific Research. 2021; 09 (A):42957-42958 doi:10.24327/ijrsr.2021.1209.6184
- Vetcher AA, Zhukov KV, Gasparuan BA, Shishonin AY. Restoration of HbA1c level for pre-diabetic patients through the restoration of arterial blood flow access to rhomboid fossa Diabetology. 2022; 3:470–476. Doi: 10.3390/diabetology3030035
- Zhukov KV, Vetcher AA, Gasparuan BA, Shishonin AY. Alteration of Relative Rates of Biodegradation and Regeneration of Cervical Spine Cartilage through the Restoration of Arterial Blood Flow Access to Rhomboid Fossa: A Hypothesis. Polymers (Basel). 2021 Dec 3;13(23):4248. doi: 10.3390/polym13234248. PMID: 34883749; PMCID: PMC8659970.
- Quynh Duong H, Maugham-Macan M. Fracture risk in breast cancer: Does obesity have an effect? A scoping review. J Bone Oncol. 2022 Aug 1;36:100449. doi: 10.1016/j.jbo.2022.100449. PMID: 35968257; PMCID: PMC9364019.
- Lujan HL, DiCarlo SE. "Seeing red" reflects hemoglobin's saturation state: a discovery-based activity for understanding the science of pulse oximetry. Adv Physiol Educ. 2022 Sep 1;46(3):461-467. doi: 10.1152/advan.00093.2022. Epub 2022 Jun 27. PMID: 35759527.
- Chan ED, Chan MM, Chan MM. Pulse oximetry: understanding its basic principles facilitates appreciation of its limitations. Respir Med. 2013 Jun;107(6):789-99. doi: 10.1016/j.rmed.2013.02.004. Epub 2013 Mar 13. PMID: 23490227.
- Shishonin AY, Zhukov KV, Gasparuan BA, Vetcher AA pH value of blood: should it be considered as a part of standard blood biochemical profile? Advance Research in Organic and Inorganic Chemistry (in press). 2022.
- Courtine G, Bunge MB, Fawcett JW, Grossman RG, Kaas JH, Lemon R, Maier I, Martin J, Nudo RJ, Ramon-Cueto A, Rouiller EM, Schnell L, Wannier T, Schwab ME, Edgerton VR. Can experiments in nonhuman primates expedite the translation of treatments for spinal cord injury in humans? Nat Med. 2007 May;13(5):561-6. doi: 10.1038/nm1595. PMID: 17479102; PMCID: PMC3245971.
- Geissler SA, Schmidt CE, Schallert T. Rodent Models and Behavioral Outcomes of Cervical Spinal Cord Injury. J Spine. 2013 Jul 27;Suppl 4:001. doi: 10.4172/2165-7939.S4-001. PMID: 25309824; PMCID: PMC4191831.
- Simon FH, Erhart P, Vcelar B, Scheuerle A, Schelzig H, Oberhuber A. Erythropoietin preconditioning improves clinical and histologic outcome in an acute spinal cord ischemia and reperfusion rabbit model. J Vasc Surg. 2016 Dec;64(6):1797-1804. doi: 10.1016/j.jvs.2015.10.011. Epub 2015 Nov 21. PMID: 26610640.
- Uezu T, Koja K, Kuniyoshi Y, Miyagi K, Shimoji M, Arakaki K, Yamashiro S, Mabuni K, Senaha S. Blood distribution to the anterior spinal artery from each segment of intercostal and lumbar arteries. J Cardiovasc Surg (Torino). 2003 Oct;44(5):637-45. PMID: 14735053.
- Singh VK, Thrall KD, Hauer-Jensen M. Minipigs as models in drug discovery. Expert Opin Drug Discov. 2016 Dec;11(12):1131-1134. doi: 10.1080/17460441.2016.1223039. Epub 2016 Aug 22. Erratum in: Expert Opin Drug Discov. 2017 Jul;12 (7):755. PMID: 27546211.
- Maršala M. Spinal cord blood flow and metabolism in transient spinal ischemia. In: E Stålberg, HS Sharma, Y Olsson, editors. Spinal cord monitoring. New York: Springer. 1998; 5-25.
- Pais D, Casal D, Arantes M, Casimiro M, O'Neill JG. Spinal cord arteries in Canis familiaris and their variations: implications in experimental procedures. Braz J Morphol Sci. 2007; 24: 224-228.
- DeGirolami U, Zivin JA. Neuropathology of experimental spinal cord ischemia in the rabbit. J Neuropathol Exp Neurol. 1982 Mar;41(2):129-49. doi: 10.1097/00005072-198203000-00004. PMID: 7062084.
- National Research Council (US) Committee on Scientific and Humane Issues in the Use of Random Source Dogs and Cats in Research. Scientific and Humane Issues in the Use of Random Source Dogs and Cats in Research. Washington (DC): National Academies Press (US); 2009. PMID: 20662127.